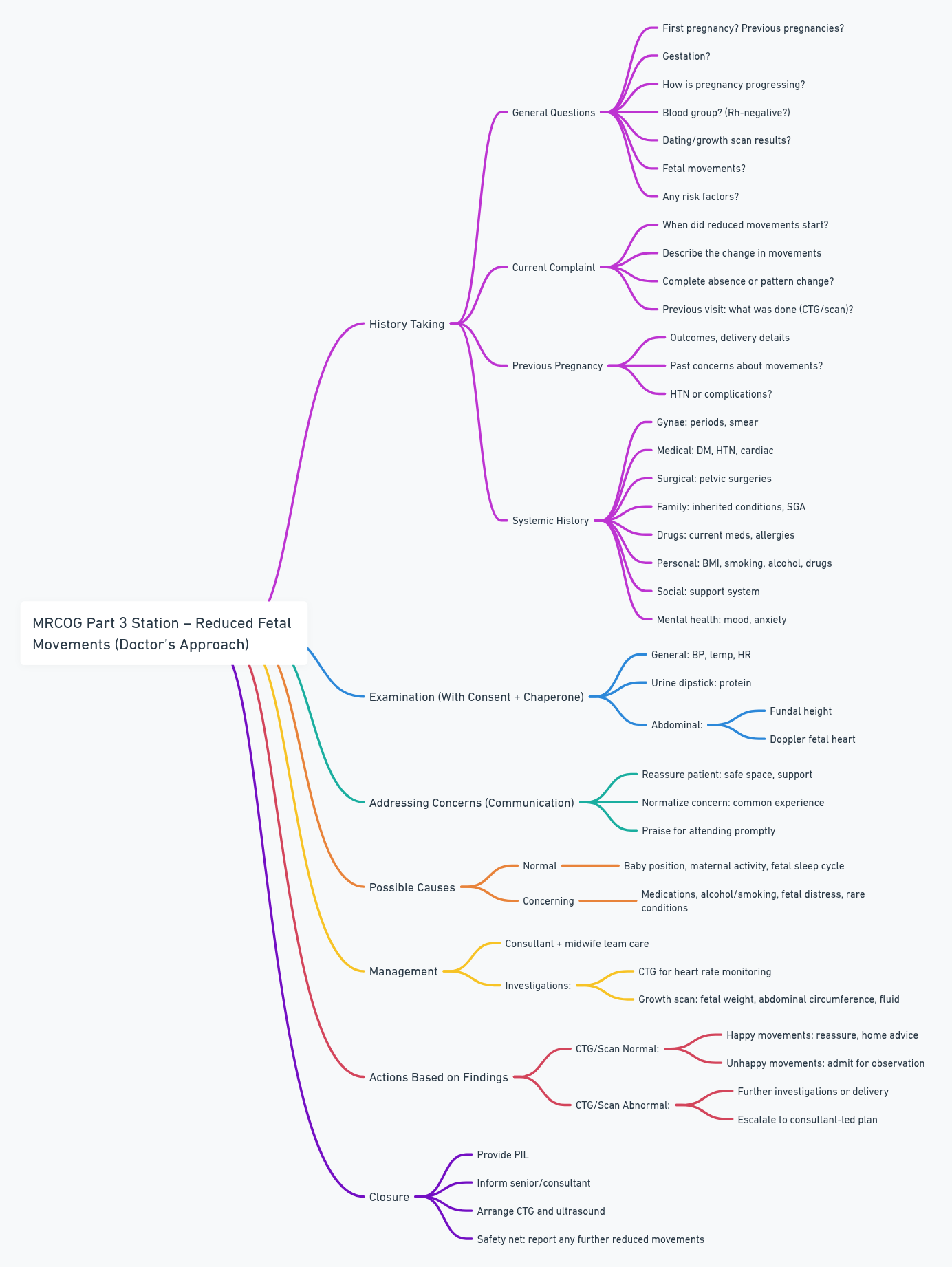
Reduced fetal Movements
Simulated patient task assessing the following clinical skills:
- Patient safety
- Communicating with patients and families
- Information gathering
- Applied clinical knowledge
Scenario:
You are the ST5 in A&E, and you’ve been tasked to consult with Sarah Mitchell, a 25-year-old woman, pregnant 33 weeks in her second pregnancy.
She reported that she has reduced baby movement, and this is her second visit to A&E because of this problem.
You have 10 minutes during which you are expected to:
- Obtain a brief, targeted clinical history
- Justify a management plan
- Answer the patient’s questions
Discussion & Questions
History
General Questions:
- Is this your first pregnancy? Any previous pregnancies?
- Duration of pregnancy?
- How is the pregnancy going?
- Blood group? (Rh-negative – take into account)
- Dating and growth scans?
- Any concerns about fetal movements?
- Any known risk factors?
Current Complaint:
- When did you first notice reduced movements?
- Can you describe what you mean by “reduced movements”?
- Pattern change or complete absence?
- What happened during your first visit for this complaint?
- Any tests done (CTG, scan)? What were the results?
Previous Pregnancy:
- Outcome and delivery?
- Similar concerns before?
- HTN or other complications?
Systemic History:
- Gynae: Periods, smears?
- Medical: DM, HTN, heart disease?
- Surgical: Any pelvic surgeries?
- Family: Inherited conditions, SGA risks?
- Drugs: Any current meds or allergies?
- Personal: BMI, smoking, alcohol, drug use?
- Social: Support systems?
- Mental Health: Mood, depression, anxiety?
Examination
- With consent and a chaperone:
- General: BP, temp, HR
- Urine dip: Check protein
- Abdominal exam:
- Fundal height (growth)
- Fetal heart with handheld Doppler
Addressing Concerns (Reassurance)
- “You’re in a safe place with us; we are here to help.”
- “It’s common to feel worried about reduced movements.”
- “You did the right thing by coming in.”
- “We’ll keep you updated and involved throughout.”
Possible Causes
Normal Factors:
- Baby’s position (back/anterior placenta)
- You being active
- Baby asleep (up to 20–40 min)
Concerning Causes:
- Medications (pain relief, sedatives)
- Alcohol/smoking
- Fetal distress or neurological/muscle conditions (rare)
Management
Care:
- Under consultant and midwifery team
Investigations:
- CTG – to monitor fetal heart rate
- Growth Ultrasound – check:
- Abdominal circumference
- Fetal weight (SGA)
- Amniotic fluid volume
Actions Based on Results:
| CTG/Scan Status | Happy with Movements | Unhappy with Movements |
|---|---|---|
| Normal | Reassure + home advice | Admit for observation |
| Abnormal | Further investigations / delivery? | Consultant-led care, escalate plan |
- Warning: Report immediately if reduced movements recur.
Closure
- Provide PIL (Patient Information Leaflet)
- Inform senior/consultant
- Arrange CTG + Ultrasound